Home / Neck, Submandibular Thyroid & Parotid Gland / Parotid Tumours
Parotid Tumours
Call +65 8125 3580
for 24 by 7 appointment
What are parotid tumours?
Among the salivary glands that we have, the parotid glands are the largest. There are two parotid glands one on each side. Located in front of the ears, these glands extend down to the upper part of the neck. The glands secrete saliva that is carried through a duct that opens on the inner surface of the cheek adjacent to the second upper molar. Just like in any other part of the body, the parotid glands may develop abnormal growths or tumours. A wide variety of tumours may occur within the parotid glans but the majority, more than 80%, are benign. Among the benign tumours, the commonest is PLEOMORPHIC ADENOMA. Some of the benign tumours like the pleomorphic adenomas can be potentially malignant. Malignant tumours of the parotid gland are of several types and their behaviour may vary from being low grade, moderate or high grade malignancy. The parotid gland also contains tissue that is non-parotid in origin. This includes lymph nodes, nerves and vessels. Growth involving these structures may also masquerade a parotid tumour.
Presentation
Patients with a parotid tumour typically present with a swelling around or just below the ear lobule. This swelling may be vary in size and consistency.
Diagnosis
The diagnosis is established from a detailed history, examination and a high index of suspicion. When a parotid tumour is suspected some investigations are done to confirm the diagnosis.
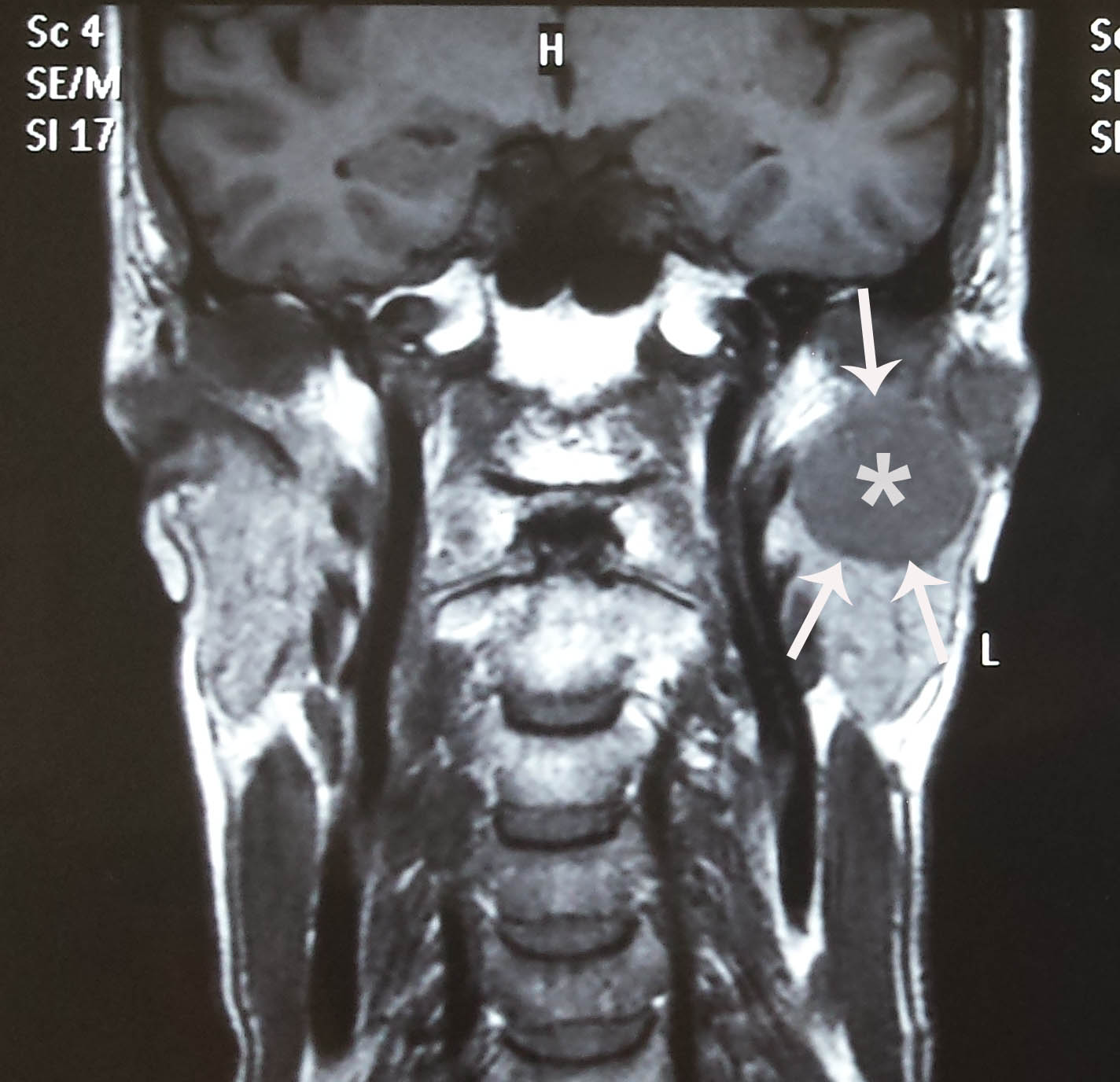
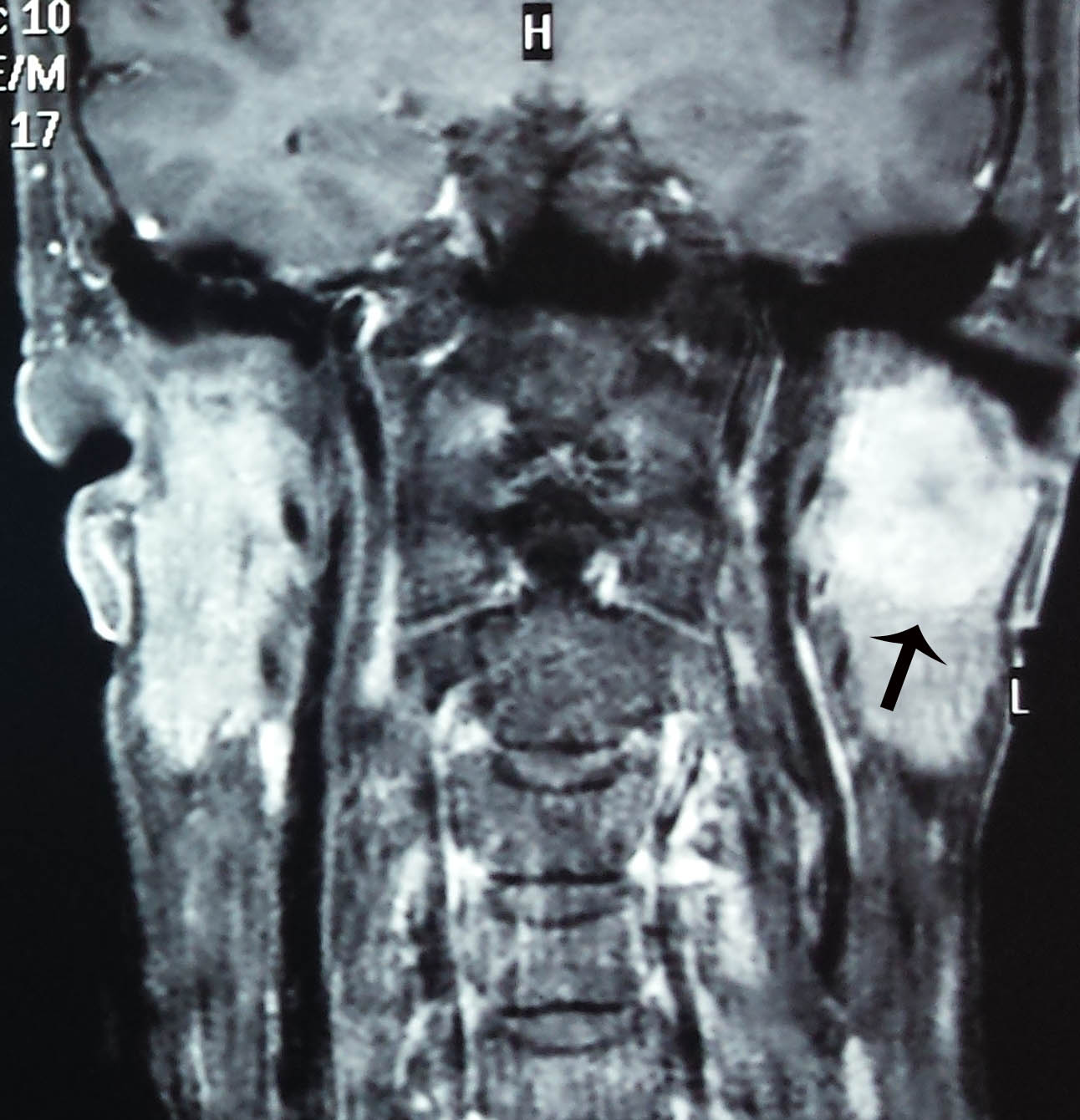
These include imaging studies such as CT or MRI scan and a fine needle aspiration. Imaging studies provide information regarding the size and extent of the tumour which is useful in planning the surgery. Fine needle aspiration involves aspirating some cells from the tumour which in some cases may provide information of the cell-type of the tumour. As there are many types of tumours that can originate in the parotid gland a pre-operative diagnosis is of the cell-type is very useful in planning surgery.
Pleomorphic Adenoma
Pleomorphic adenoma is the commonest tumour of the parotid gland. ( Pleo = many, morphic = forms, adenoma = benign tumour) Literally pleomorphic adenoma means a “benign tumour that may have several forms”. Though the tumour is benign and slow growing, it is potentially malignant and needs to be completely removed. It also has a tendency to recur unless it is completely removed with a wide margin.
Treatment
The standard treatment for parotid tumours is surgery which involves removal of part or whole of the parotid gland. In some situations, where the fine needle aspiration had not been diagnostic removal of the tumour also provides a histological diagnosis. A complete removal of the tumour is sufficient for most benign parotid tumours. Malignant parotid tumours may require additional treatment such as radiotherapy/chemotherapy.
How is parotid gland surgery done?
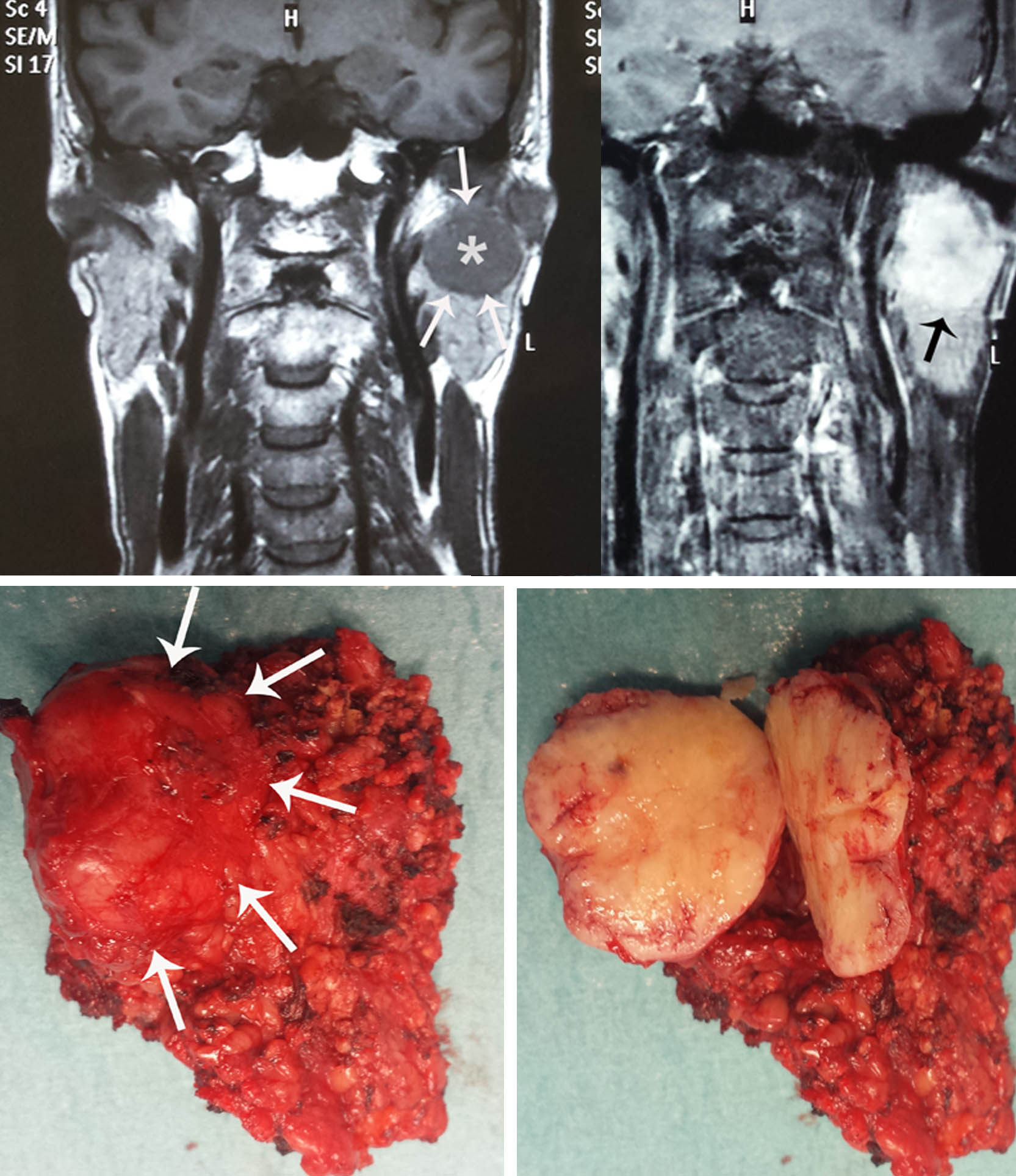
A large pleomorphic adenoma seen on the MRI scan. The tumor has been cut open on the surgical specimen below. The white arrows on the surgical specimen point to the tumour. A superficial parotidectomy was done.
The parotid gland is arbitrarily divided into two lobes. The superficial lobe, which is superficial to the facial nerve, that runs through the gland and the deep lobe which is deep to the nerve. As most parotid tumours originate in the superficial lobe surgery involves removal of the superficial lobe of the parotid gland along with the tumour. This is called SUPERFICIAL PAROTIDECTOMY. When the deep lobe is involved the entire parotid gland must be removed and the surgery is called TOTAL PAROTIDECTOMY. The surgery is carried out under general anesthesia. An incision extending from the front of the ear to just behind the ear and upper neck is required. The incision usually heals very well and the scar is barely perceptible after a few months. One of the sensory nerves (greater auricular nerve) has to be divided during the surgery and this result in temporary or often permanent numbness over the scar. Another nerve that may be occasionally inadvertently traumatized is the facial nerve that supplies that part of the face. This nerve runs within the gland and injury to the nerve may result in partial paralysis of that part of the face. The operation may take two to two and half hours. A small tube is usually left inside the wound for 2-3 days. As the incision is closed and is almost watertight any oozing within the wound may accumulate and cause the blood to collect in the wound. This is called a hemotoma. The tube that is inserted drains the blood preventing hemotoma formation. Some pain and nausea is common after the operation. Appropriate medications are given postoperatively to counter this. Antibiotics are given to avoid infection. The patient may be required to stay in the hospital for 2-3 days after the operation. Once the drainage from the drain is minimal it can be removed and the patient can be discharged. Post- operative instructions are given on discharge. The stitches are removed in about a week by when the wound union has taken place. Complications of parotidectomy in addition to explained above include infection, hemotoma, bleeding, damage to the parotid duct with resultant salivary fistula, and excessive sensitivity over the cheek especially during meals ( Frey’s syndrome).
What is the facial nerve? How is it related to parotid surgery?
The facial nerve is the 7th of the twelve cranial nerves. Though it has some sensory supply to some structures it mainly supplies the muscles of the face responsible for facial expression. Injury to this nerve will result in paralysis of that side of the face resulting in facial asymmetry and inability to close the eye. As a result of the weakness or paralysis of the facial muscles the face sags and mouth becomes “crooked” when the patient smiles. As the patient is unable to close the eye or even blink, continuous exposure of the eye to air results in dryness of the eye and damage to the conjunctiva and cornea. The resulting deformity may have significant health and social implications.
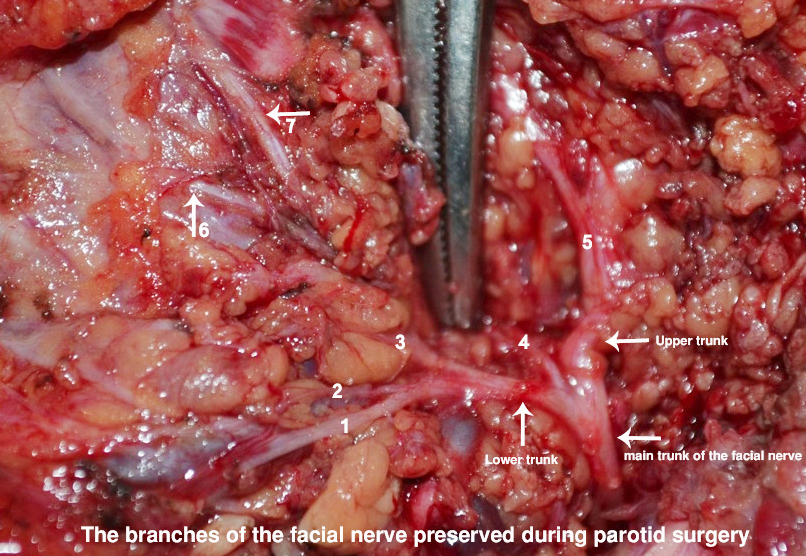
The facial nerve arises from the brain stem and passes through a foramen located next to the inner ear and it enters the middle ear. It exits the ear just below the ear and deep to the angle of the jaw. It then enters the parotid gland. The main trunk of the nerve then divides into an upper and lower branch and subsequently divides into five branches which supply the muscles of the face.
To avoid injury to the nerve during the surgery it must be identified and all branches protected. Very meticulous dissection and good surgical skills are required.
What is superficial parotidectomy?
Most parotid tumours are superficial to the facial nerve and therefore require removal of the parotid gland that is superficial to it. The surgery is called SUPERFICIAL PAROTIDECTOMY. No manipulation or mobilisation of the nerve is necessary in these cases.
What is total parotidectomy?
Some tumours may arise from the parotid tissue that is deep the nerve.In such cases some branches of the nerve may have to be retracted and mobilised to be able to remove the tumour deep to the nerve. As both the superficial and deep lobe are removed the surgery is called TOTAL PAROTIDECTOMY. Some weakness of the facial muscles may result from the manipulation of the nerve. It is often temporary.
Not sure which treatment is you? Speak to A/Prof Sethi to find out if this is the right treatment for you at +65 8125 3580. Or book an appointment with A/Prof Sethi for a consultation on your symptoms and treatment options.
